Many people think a plugged duct is caused by a backup of thickened milk but the plugging comes from outside the duct.
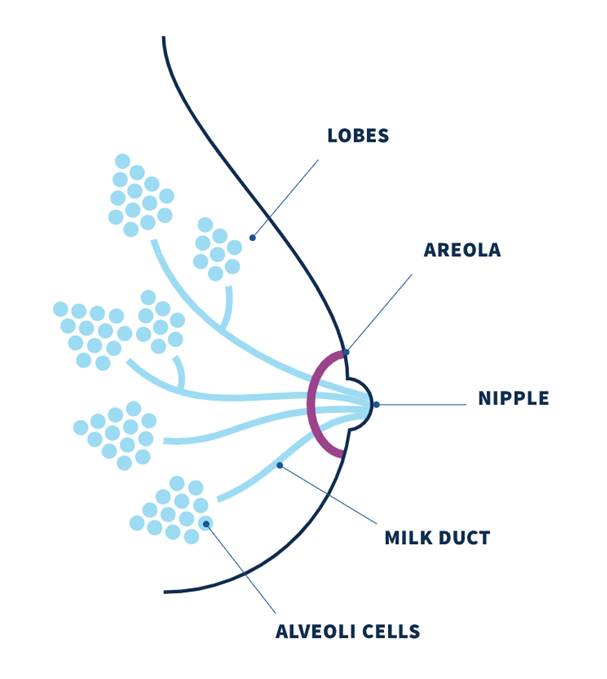
Our milk ducts carry milk from the milk making cells which are grouped together in alveoli. The alveoli are like little clusters of grapes which connect to the ducts. The ducts carry milk to the nipple openings.
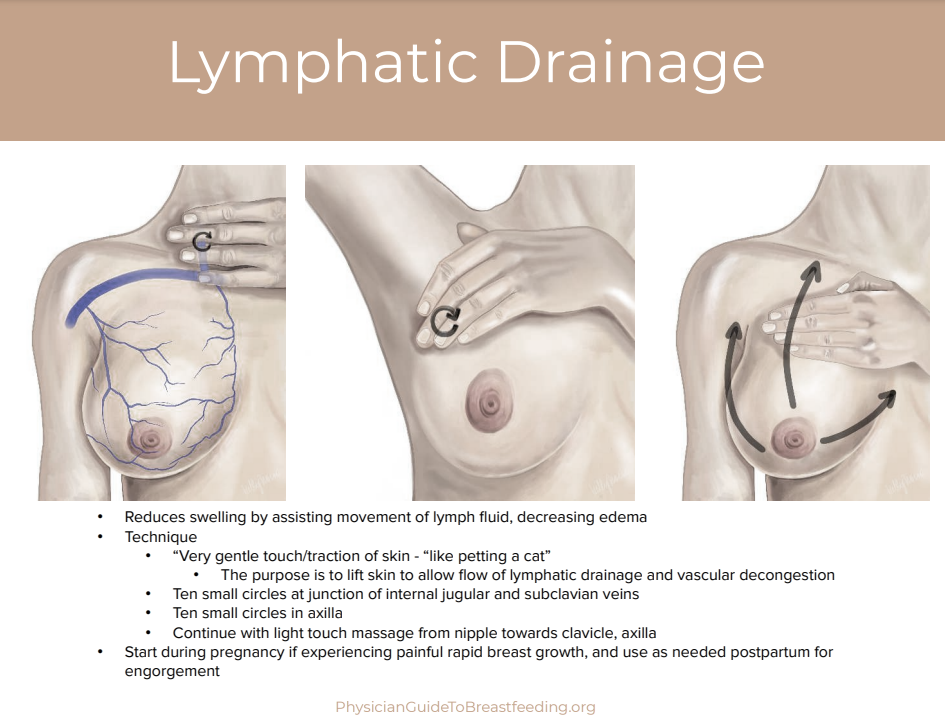
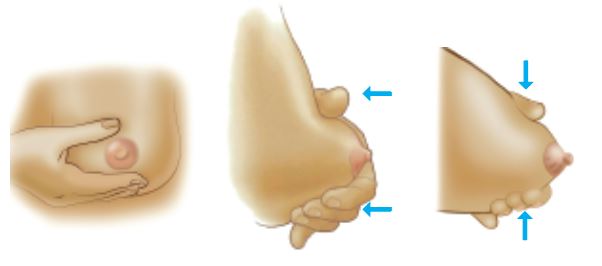
A breast “plug” represents an area of swelling in the breast and more accurately reflects lymphatic fluid congestion and dilated capillaries than a “plug of milk.” The plugging is caused by engorgement and congestion of fluid and blood vessels pressing in on the duct from outside which narrows the pathway.
Exclusive or excessive pumping, nipple shield use, oversupply, unresolved engorgement, inflammation, or subacute mastitis increases plugging.
To treat plugging, try the following:
- Warmth before feeding. A warm shower or warm pack applied to the breast.
- Ibuprofen and/or Tylenol as needed along with a cool pack applied after feeding/pumping.
- Avoid massage and excessive pumping (remember it’s not milk that’s plugged).
- 5-10 grams daily oral sunflower lecithin supplementation
This should resolve in 24hrs. If it does not, contact your provider and lactation consultant for guidance. Therapeutic ultrasound is very effective. Your doctor may prescribe a single dose of 10-30mg of Pseudoephedrine (Sudafed) which acts as a vasoconstricting agent (i.e. decreases blood flow) and may help with any pain.
Any plug or mass persisting for several days and not resolving with conservative interventions requires referral to a medical provider, who may obtain breast imaging to rule out galactocele and/or other mass.