Wow! It was so amazing to see you all and celebrate the special relationship we share with our babies and community!



















Wow! It was so amazing to see you all and celebrate the special relationship we share with our babies and community!



















Choline is an essential nutrient during pregnancy and lactation but only 15% of us are getting the recommended daily amount.
So what is it and why do we need it?

Choline is one of the many B Vitamins we need. B4, to be exact.
Choline is a key nutrient for fetal brain development and protection. Choline supports brain development, memory, and learning —and protects us from infections. When we think about brain development during fetal growth we often think about folate (which is also very important!) but choline plays an important role in neural tube development.
During pregnancy choline protects us from serious complications.
Choline is required for maintaining normal levels of homocysteine:
Elevated homocysteine levels during pregnancy have been associated with complications like: preeclampsia, miscarriage, placental abruption, intrauterine growth restrictions (IUGR) , venous thrombosis, and cardiovascular related complications.
Adequate choline during pregnancy can also protect us from cholestasis which is a common complicating during pregnancy and postpartum.
Choline can also be used to reduce risks and prevent mastitis. It is one of the components of lecithin.
Choline RDA During pregnancy 450 mg/day During lactation 550 mg/day
Choline is a naturally occurring amino acid found in egg yolks, liver, animal meat, beans, milk, some vegetables, as well as in human breast milk.
Amount of Choline Per Serving of Food:
If you are considering supplementing your diet with choline look for products containing phosphatidylcholine.
❤ Megan
“The American Academy of Pediatrics (AAP) recommends exclusive breastfeeding for about the first six months. We support continued breastfeeding after solid foods are introduced as long as you and your baby desire, for 2 years or beyond.”

The new recommendations bring the AAP in line with the World Health Organization, UNICEF, The American Academy of Family Physicians, and so many more health organizations!
This article from Healthy Children explains the recommendations and highlights the need for skilled lactation support. It also addresses the structural barriers to meeting these feeding goals.
You can read the official statement titled “Breastfeeding and the Use of Human Milk” here.
❤ Megan

The Basics of Inducing Lactation — Breastfeeding Without Birthing (Alyssa Schnell, IBCLC)
Milk Junkies — Breastfeeding and parenting from a transgender perspective (Trevor MacDonald)
Using an At-Chest Supplement Device
Trans Breastfeeding FAQ – Diana West
Find an LGBTQ Care Provider — Breastfeeding Network (Jaye Simpson, IBCLC)
Professional Organizations on LGBT Parenting — Human Rights Council
Two Women and a Baby: LGBTQ and Breastfeeding
❤ Megan
Even the name is foreboding and for good reason! (NEC) is a serious gastrointestinal problem that mostly affects the intestines premature babies. This inflammatory condition can happen when infants are not receiving only human milk or have received antibiotics which can cause damage in the digestive tract.
May is Necrotizing Enterocolitis Awareness Month
There is a ton of research which looks at the connection between human milk feeding and significantly reducing the risk of developing NEC.
To learn more check out NEC Society
“Nipple thrush pain is often described as burning, itching, or stinging and may be mild to severe. The pain is usually ongoing and doesn’t go away with improved positioning and attachment of your baby to the breast.”
“When you have nipple thrush, your nipple appearance may change to being shiny in appearance, sometimes chapped, blistered with white patches but may also look completely normal. You may also experience itchy, flaky and red nipples or areola.”

Thrush is an overgrowth of candida or yeast. It mostly commonly causes an infection and overgrowth in people who are immunocompromised. It can overgrow in areas with skin folds which are moist and warm, like armpits, the vagina, etc. It’s very rare to have yeast/candida/thrush in highly vascularized areas like the breasts and nipples.
Research has shown that in cases of suspected thrush the parent is most likely experiencing mastitis
“microbiological analysis of milk samples provided by 529 women with symptoms compatible with “mammary candidiasis”. Nipple swabs and nipple biopsy samples were also collected… Results showed that the role played by yeasts in breast and nipple pain is, if any, marginal…our results strongly support that coagulase-negative staphylococci and streptococci are the agents responsible for such cases.“
When providers visually assess for thrush, they may be seeing dermatitis rather than a yeast overgrowth on the nipples. Dermatitis is an allergic reaction or irritation caused by something the parent is sensitive to on their skin. This can include creams, ointments, and medications.
Here are some pictures of parents who thought they had thrush but actually had dermatitis!


Below, is what yeast on the skin actually looks like

So what you should you do if you think you have thrush?
Talk to your Lactation Consultant for a full feeding and breast evaluation. They can make referrals to providers for treatment, if needed, and can help figure out what’s actually going on!
❤ Megan
March 22-28 is a time to be grateful for all that doulas provide to us during pregnancy, birth, and beyond!

A doula is a professional labor assistant who provides physical and emotional support to you and your partner during pregnancy, childbirth and the postpartum period.
Did you have a doula?
How was your experience supported by your doula?

Doulas can support breastfeeding in lots of ways!
By teaching basic hold and latch techniques.
By discussing your feeding options and helping you sort out what’s right for you.
By helping you to have a healthy and safe birth so you can get started with the Golden Hour right away!
By providing education, encouragement, and resources to help you keep breastfeeding if you run into any bumps.
By connecting you to other knowledgeable providers who can assist and support you.
Thank your doula today!
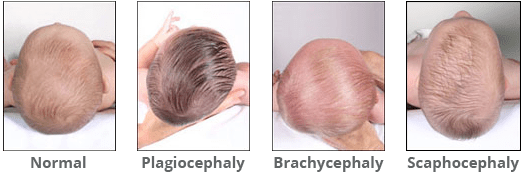
March marks Plagiocephaly and Torticollis Awareness Month.
Plagiocephaly is when a baby develops a flat spot on one side or the back of the head. It happens when a baby sleeps in the same position most of the time or because of problems with the neck muscles that result in a head-turning preference.
In babies, torticollis happens when the muscles that connect the breastbone and collarbone to the skull (sternocleidomastoid muscle) are shortened.
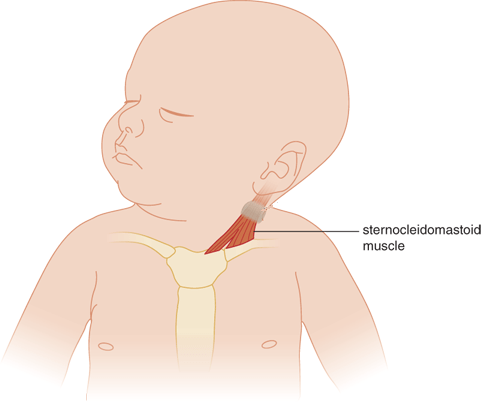
There are many reasons that babies can develop these conditions and none of them are your fault! In fact, plagiocephaly and torticollis are becoming increasingly common.
Here are some reasons your baby may have one or both of these conditions:
The good news is that you can treat both of these conditions! Working with a pediatric PT is very helpful!
At home you can do fun activities with your baby to help them develop and improve.

With help and time, it will get better and you are likely to see big improvements in your baby’s feeding, too!
❤ Megan

Does your baby gag, choke, and cough during feeding? Are they sputtering and tugging on your breast? Ever notice them clicking or leaking milk? What about gas…do they seem to have an awful of it?
There could be a number of things causing baby to struggle with feeding.
Let’s learn about the differences.

Strong MER
Inside your breast are milk making cells that form a sphere. These spheres are clustered together so I like to think of them as bunches of grapes with the stems representing the ducts that carry milk to the nipple.
Each grape is wrapped with muscle fibers. When your baby is feeding (or sometimes just when you think about your baby!) your oxytocin rises. Oxytocin is a hormone which plays a role in bonding, pleasure, and MER. It’s the same hormone that kicks starts uterine contractions during birth. The muscle fibers respond to oxytocin and squeeze milk down the ducts and out the nipple.
To have strong MER you need strong muscle contractions. Over the first 3 months, MER starts to chill out because those little squeezing muscles become less sensitive to it.
Oversupply
We actually just talked about oversupply. If you have an oversupply, when the muscles contract the milk making “grapes” are soo full that milk flows very quickly.
Ineffective Latch
Latch, or attachment to the breast, can be ineffective due to positioning, other medical conditions, tongue tie, or due to something else.

Hmmm, I think I know what’s going on. What do I do about it?
Make an appointment with your Lactation Consultant so they can give you personalized instruction and make a plan which will work for you!
All too often, the difficulty is with your baby and not with you. Your IBCLC can direct you to care which can include changing your feeding plan, adjusting your position, suck training exercises, working with a physical/occupational therapist, or SLP.
We are here to help!
❤ Megan
Many people think a plugged duct is caused by a backup of thickened milk but the plugging comes from outside the duct.
Our milk ducts carry milk from the milk making cells which are grouped together in alveoli. The alveoli are like little clusters of grapes which connect to the ducts. The ducts carry milk to the nipple openings.
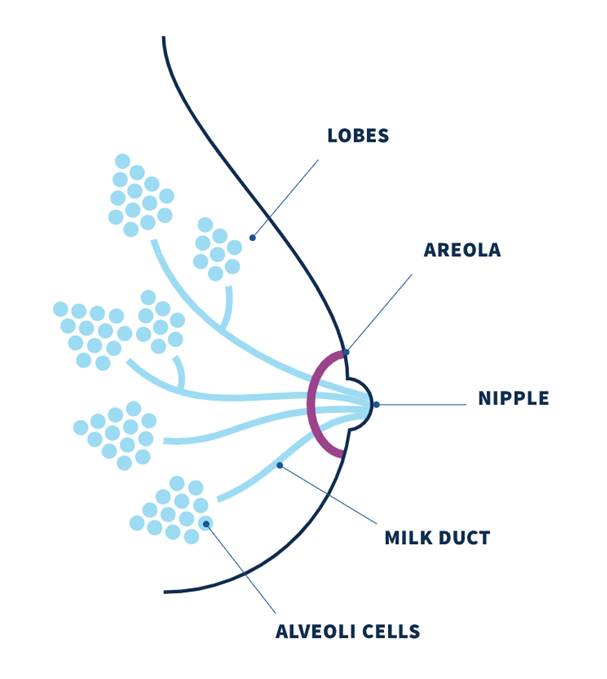
A breast “plug” represents an area of swelling in the breast and more accurately reflects lymphatic fluid congestion and dilated capillaries than a “plug of milk.” The plugging is caused by engorgement and congestion of fluid and blood vessels pressing in on the duct from outside which narrows the pathway.
Exclusive or excessive pumping, nipple shield use, oversupply, unresolved engorgement, inflammation, or subacute mastitis increases plugging.
To treat plugging, try the following:
This should resolve in 24hrs. If it does not, contact your provider and lactation consultant for guidance. Therapeutic ultrasound is very effective. Your doctor may prescribe a single dose of 10-30mg of Pseudoephedrine (Sudafed) which acts as a vasoconstricting agent (i.e. decreases blood flow) and may help with any pain.
Any plug or mass persisting for several days and not resolving with conservative interventions requires referral to a medical provider, who may obtain breast imaging to rule out galactocele and/or other mass.